Sacral neuromodulation, or sacral nerve stimulation (SNS), treats bladder and bowel conditions like overactive bladder, urinary retention, urgency urinary incontinence, and fecal incontinence.
How Sacral Neuromodulation Works
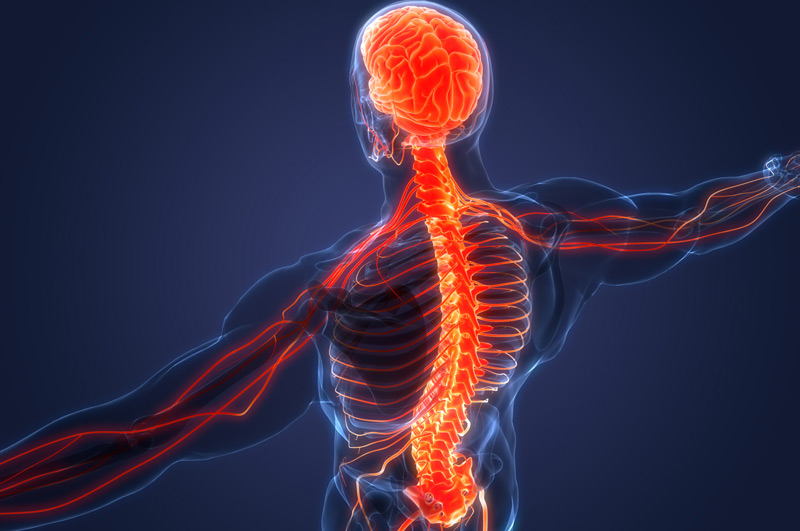
An implantable neurostimulator sends mild electrical signals to a nerve just above the tailbone, affecting the muscles and nerves that control urinary and bowel functions and communicate with the brain.
This treatment modifies the function of the sacral nerves and the signals sent to the brain about bladder and bowel sensations.
Who Needs Sacral Neuromodulation?
Patients with overactive bladders (OAB), particularly as they age, experience frequent and urgent urination, and in some cases, urgency leakage. Others may develop a bladder that ceases to function, leading to urine retention. These symptoms can also result from recent, unrelated surgery. Other conditions treated with sacral neuromodulation include:
- Spinal Cord Injury: Patients with more than 50 percent motor function who can still walk
- Multiple Sclerosis: Patients who can walk well may benefit from sacral neuromodulation

The Evaluation Phase
A thin temporary wire is inserted near the sacral nerves in the lower back, close to the tailbone. This wire connects to a small external device that delivers electrical stimulation to the nerves. The procedure takes less than an hour, after which the patient goes home to resume daily activities and keep a new diary of their toilet habits for one week.
After one week of home evaluation, the patient will have a follow-up appointment to discuss the results and determine if they are a suitable candidate for the treatment. Based on improvements, quality of life assessments, and patient satisfaction, the patient may receive an implanted device.
The Implant Phase
Patients approved for device implantation will undergo a procedure where the neurostimulator is placed above the buttocks and connected to the implanted wire. They will receive a small hand-held controller to adjust the level of stimulation.
The battery lasts between five to ten years, and the controller indicates when it needs replacement. The wire usually doesn’t need replacement or adjustment.

What to Expect During the Procedure
For the test-phase implantation, the patient will receive anesthesia and lie on their stomach. They may be asked to describe sensations, such as pulling, tingling, or tapping in their pelvic muscles and vaginal area during sacral nerve stimulation.
A small wire will be attached to the lead and exit through a small incision in the lower back.
The implant procedure is similar to the initial operation, typically done one to two weeks later. Under anesthesia, the surgeon makes a two-inch incision above the buttocks to insert the neurostimulator, which is then connected to the previously implanted wire.
Potential Risks
Sacral neuromodulation, like any procedure, carries certain risks and side effects, including:
- Swelling
- Bleeding
- Bruising
- Infection
- Device-related issues
- Pain at the implant site
- Discomfort during stimulation
- Changes in urinary or bowel function
Choose UCI Pelvic Health Center
Contact UCI Pelvic Health Center for treatment with sacral neuromodulation. Our experienced team can help manage bladder and bowel conditions, improving your quality of life with personalized care and advanced medical solutions.

