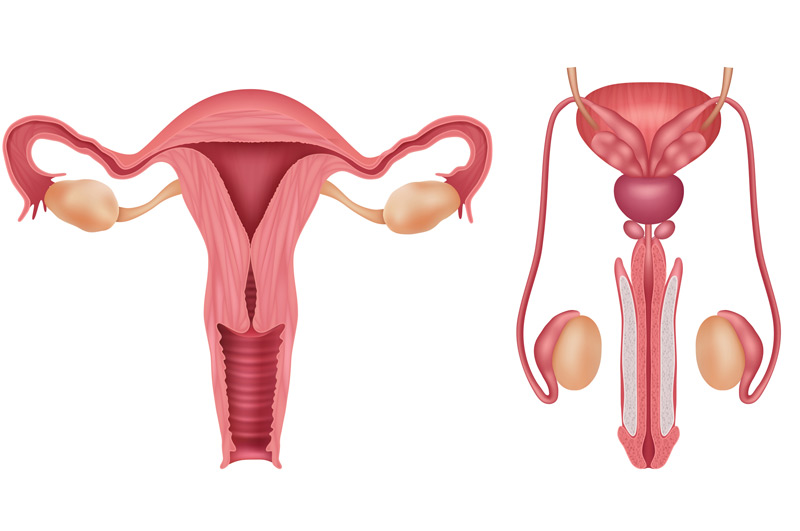
Gender affirming surgery is a category of procedures performed to assist patients while they physically transition to the gender they identify with. It is a multi-disciplinary approach that can include urologic procedures combined with Urogynecologic surgery, top surgery, and facial surgery.
The surgical transgender care provided for patients is as unique as one patient to the next, which makes it important to select a doctor who values a personalized approach when it comes to helping patients achieve a higher quality of life. It is common for patients to need more than one procedure.
Assigned Male at Birth (AMAB) Surgery
Transgender women (assigned male at birth, or AMAB) might opt for procedures such as:
- Clitoroplasty: Reconstruction of a clitoris from existing tissue
- Vaginoplasty and vulvoplasty: Construction of a vagina and labia
- Orchiectomy: Removal of the testicles
- Penectomy: Removal of the penis

Assigned Female at Birth (AFAB) Surgery
Transgender men (assigned female at birth, or AFAB) might opt for procedures such as:
- Complete vaginectomy: Removal of the entire vagina
- Hysterectomy: Removal of the uterus
- Metoidioplasty: Construction of a penis from enlarged clitoris tissue
- Phalloplasty: Construction of a penis from donor site tissue
- Salpingo-oophorectomy: Removal of the fallopian tubes and ovaries
- Scrotoplasty: Construction of a scrotum
Are There Risks?
As with other medical procedures, there are risks associated with gender affirming surgeries such as bleeding, infection, and reaction to anesthesia. Additional risks can include changes to sexual sensation, trouble emptying the b ladder, recurrent urinary tract infections (UTIs), urethral fistulas, and urethral fistulas. Your doctor will discuss all potential risks with you ahead of time.

After gender affirming surgery, many patients need to wait four to six weeks to fully recover and resume regular physical activity. Maintaining follow-up appointments is a very important part of care, and you should contact your surgeon if you experience persistent pain or bleeding for more than five weeks after your surgery.
Setting Expectations
Surgery is just one aspect of transitioning and receiving gender affirming care. Other factors can include hormonal therapy and guidance with social transitioning. Be sure to communicate with your entire healthcare team for the best results.

