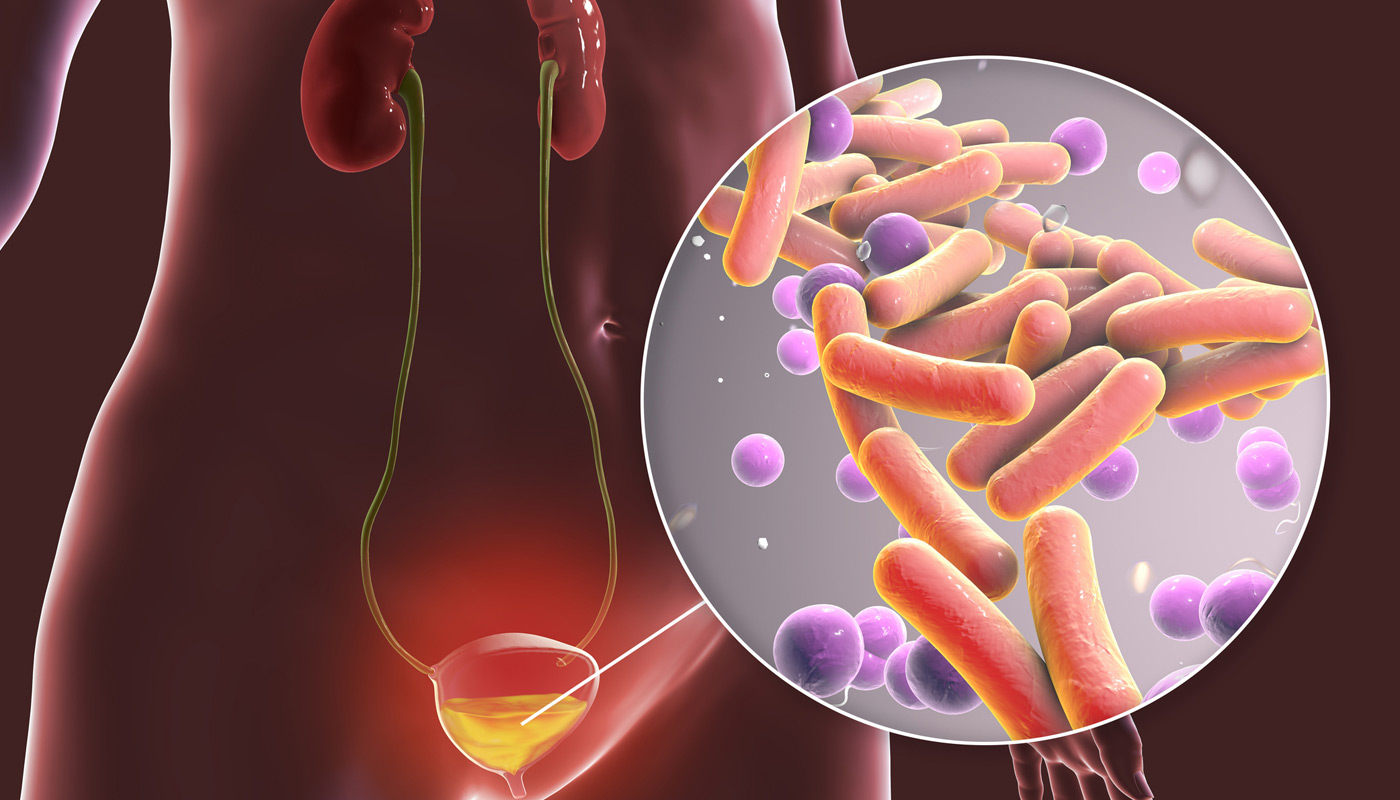
Overactive bladder (OAB) is characterized by urinary urgency that may include involuntary urine loss without a urinary tract infection or other clear causes. Approximately 11% of people globally suffer from overactive bladder.
Individuals with overactive bladder may experience frequent urination, sudden and strong urges to urinate, nocturia (frequent urination at night interrupting sleep), and urgency urinary incontinence (involuntary urine loss associated with urgency). Conditions associated with overactive bladder include:
- Urinary tract infection
- Malignancy
- Pelvic floor muscle dysfunction
- Urinary stones
- Diabetes
- Polydipsia
- Interstitial cystitis/bladder pain syndrome (IC/BPS)
- Neurogenic bladder
Risk Factors for Overactive Bladder
The likelihood of developing overactive bladder can be heightened by:
- Urinary tract infections
- Hormonal changes
- Neurological disorders or disruptions in brain-bladder signaling
- Weakness or spasms in pelvic muscles
- Medication side effects
- Diseases affecting the spinal cord or brain, such as multiple sclerosis and stroke


Diagnosis for Overactive Bladder
To diagnose overactive bladder, a physician will review the patient’s medical history, perform a physical examination, and conduct a urinalysis. At this stage, screening for conditions linked to overactive bladder, such as constipation, recurrent UTIs, pelvic floor dysfunction, pelvic organ prolapse, bladder cancer, prostate obstruction, hematuria, limited mobility, and excessive fluid/caffeine intake, is essential.
During the pelvic exam, the physician will check for pelvic floor muscle hypertonia, skin breakdown, and perineal reflexes. Women will be assessed for pelvic organ prolapse and genitourinary symptoms of menopause, while men will undergo a digital rectal exam to check for nodularity or enlargement. Urinalysis will identify any UTIs and hematuria. Additional diagnostic tools for overactive bladder may include intake-voiding diaries, post-void residual measurements, urine cultures, and validated symptom questionnaires.
Treatment for Overactive Bladder
The primary treatment for overactive bladder involves behavioral therapies, such as bladder training, fluid management, bladder control strategies, pelvic floor muscle training (PFMT), and urgency suppression.
Biofeedback, using electronic monitoring to train patients to control pelvic floor functions, can also be beneficial. Sensors assess pelvic floor muscle activity, and the physician provides feedback to guide pelvic floor physical therapy.
Secondary treatment options for overactive bladder may include medication.
Choose UCI Pelvic Health Center for Overactive Bladder Treatment
If you’re experiencing symptoms of overactive bladder (OAB), such as frequent urination, urgency, or urinary incontinence, don’t let it disrupt your life any longer. The UCI Pelvic Health Center offers specialized care and advanced treatment options to help you regain control and improve your quality of life.
Our experienced team of physicians understands the challenges OAB can pose and provides personalized care tailored to your needs, including behavioral therapies, medication management, and advanced interventions like biofeedback and pelvic floor physical therapy.

