Urinary storage and voiding dysfunction is characterized by difficulty in completely emptying the bladder during urination.
About Urinary Retention
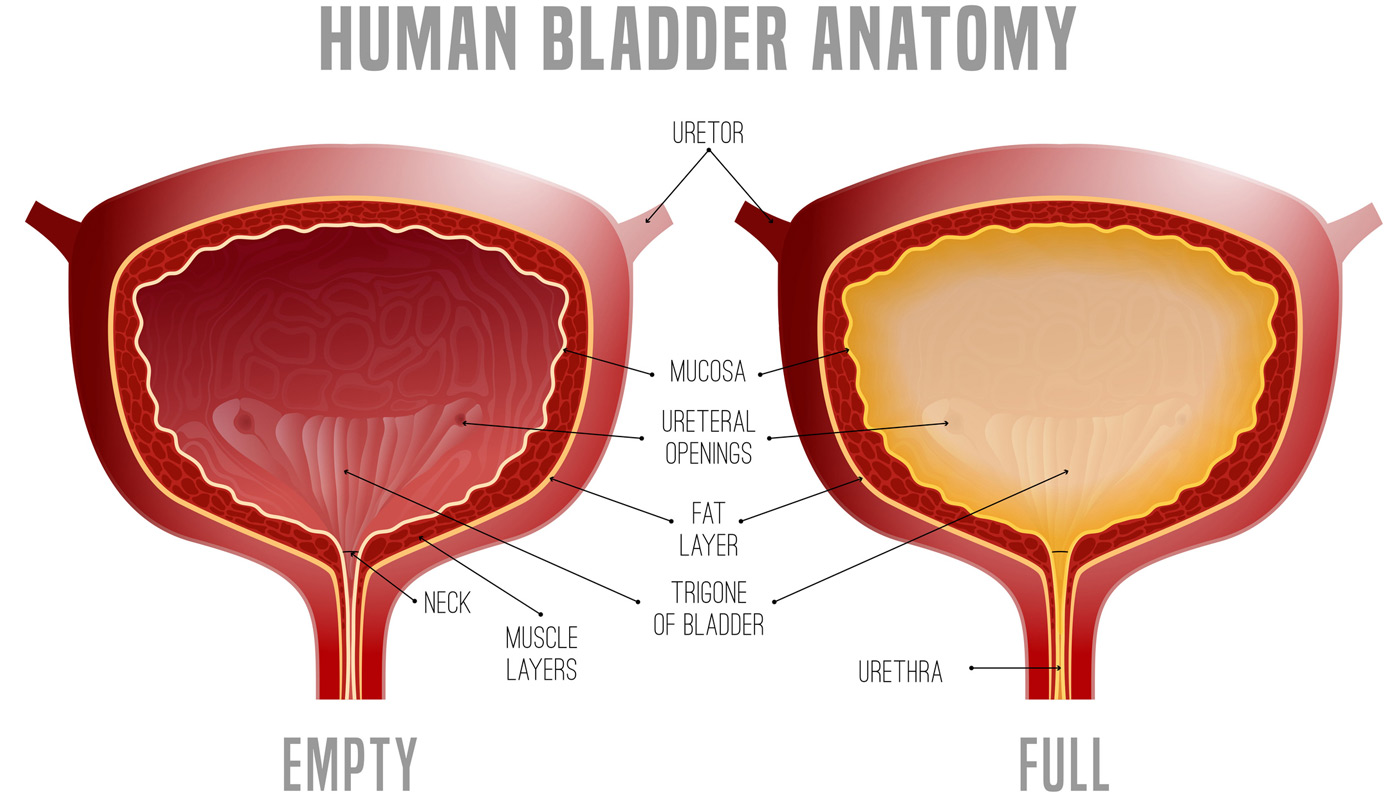
Urinary retention occurs when urine, which is filtered from the blood and stored in the kidneys, moves to the bladder but is not fully expelled through the urethra during urination. This condition can be either acute (sudden) or chronic (long-term). Acute urinary retention develops rapidly and can be severe, whereas chronic urinary retention persists over a long period.
Acute urinary retention is a medical emergency requiring immediate treatment.


Symptoms of Urinary Retention
Those with chronic urinary retention may experience symptoms such as:
- Difficulty initiating urine flow
- Urine leakage due to a full bladder
- Inability to start urination
- Weak urine stream
- Feeling the need to urinate again soon after finishing
Individuals with acute urinary retention may suddenly be unable to urinate at all or can only urinate in very small amounts, even with a full bladder.
Causes of Urinary Retention
Urinary retention can be caused by:
- Medications
- A blockage in the urinary system
- Infections and swelling that prevent urination
- Nerve problems disrupting communication between the brain and urinary system
- Complications and side effects from post-surgical medication
Diagnosing Voiding Dysfunction
During a medical appointment, the doctor will review the patient’s medical history and conduct a physical exam. Male patients will be checked for prostate issues, such as enlargement. Some patients may need to keep a bladder diary to track their urination patterns.
The following tests may be required to diagnose voiding dysfunction:
- Cystoscopy to evaluate the bladder
- Urinalysis to check for urinary tract infections
- Blood test to measure prostate-specific antigen (PSA) levels in men
- Ultrasound to determine the amount of urine remaining in the bladder after urination and identify voiding problems
- Urodynamic testing to assess the bladder’s ability to hold urine and the coordination of muscles in the bladder, urethra, and pelvis
Treatment Options for Voiding Dysfunction
Treatment for voiding dysfunction depends on the underlying cause. Common treatments include:
- Bladder Training: Teaches muscles to support the bladder, helping patients hold urine longer or urinate more easily.
- Medications: Tamsulosin can improve voiding issues, while oxybutynin and tolterodine treat urinary urgency or leakage.
- Pelvic Floor Therapy: Helps patients relax pelvic floor muscles to ease urination. Biofeedback sensors may be placed in the vagina or rectum to ensure correct muscle use during therapy.
- Botox Injections: Relax bladder muscles to treat urge incontinence.
- Sacral Nerve Stimulation: Reduces urinary urgency and leakage and helps empty the bladder more effectively. A neurotransmitter under the skin sends mild electrical impulses to the sacral nerve.
- Percutaneous Tibial Nerve Stimulation (PTNS): Improves bladder control. An electrode near the tibial nerve in the ankle is used to send mild electrical signals to the sacral nerve, which controls the bladder, urinary sphincter, and pelvic floor muscles.
- Self-Catheterization: Drains urine from the bladder.
Choose UCI Pelvic Health Center
Experience comprehensive care for urinary storage and voiding dysfunction at UCI Pelvic Health Center. Our team offers personalized treatment plans tailored to your needs, combining cutting-edge techniques with compassionate care.

