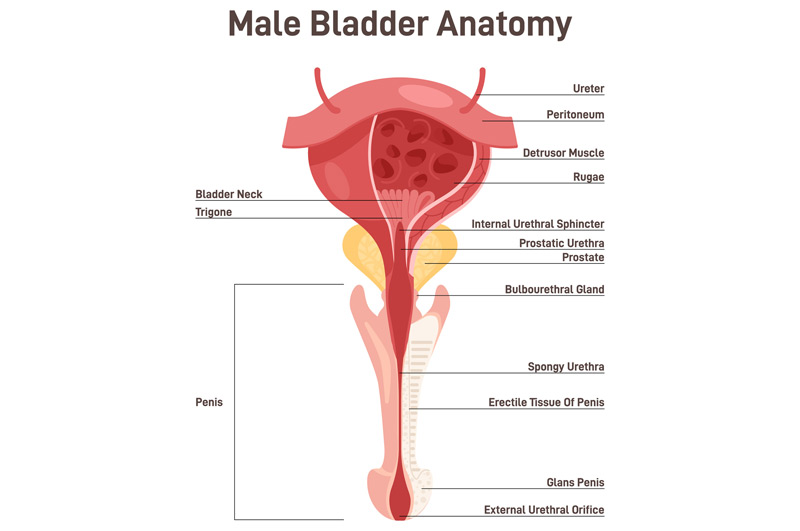
Bladder neck contracture (BNC) is a potential complication following prostate surgery, pelvic and lower urinary tract traumas or after radiation therapy to the lower genitourinary tract. Scar tissue can develop at the junction where the bladder connects to the prostate or, after prostate removal, at the junction between the bladder and urethra (known as the anastomosis).
During prostate removal surgery, the bladder neck, which was previously attached to the prostate, is reconnected to the urethra. Scar tissue forming at this connection can narrow or completely close the passage between the bladder and urethra.
Symptoms of Bladder Neck Contracture
Patients may experience symptoms of BNC within three to six months after prostate surgery. An early indicator is a gradual decrease in urine flow. Eventually, patients may be unable to urinate or experience overflow incontinence when the bladder becomes overly full.
Additional symptoms include:
- Needing to push to start urinating
- A urine stream that starts and stops
- Delays in the onset of urination after feeling the urge
- A slow or weakened urine stream
- A sensation of incomplete bladder emptying

Causes of Bladder Neck Contracture
The exact cause of BNC is unclear. One possible cause is a gap at the surgical connection site that leads to a blood clot (hematoma) or other healing issues beneath or between the stitches. As a result, the stitches can break or tear, creating scar tissue that narrows the bladder neck. Another potential cause is poor blood supply to the anastomosis, which can result from overly tight stitches cutting off blood vessels. Conditions such as diabetes and heart disease, which are associated with poor blood flow, may also contribute to BNC.
Risk Factors for BNC
Risk factors for developing BNC include:
- A history of diabetes and/or coronary artery disease
- Poor surgical technique
- Post-surgical complications such as prolonged urine leakage, hemorrhage, and anastomotic disruption
- A history of smoking
- Older age
- Obesity
- Primary cancer treatment

Diagnosing Bladder Neck Contracture
To diagnose BNC, a physician may perform a cystoscopy. This procedure involves inserting a thin instrument with a lens and light through the urethra to visualize the connection site. Local anesthesia is administered, and the cystoscope is passed into the bladder, which may be filled with sterile water or saline to improve the view. The procedure takes about two minutes. Alternatively, a cystourethrogram may be ordered to check for structural issues in the urethra or bladder. This involves inserting a urinary catheter and injecting a contrast material into the bladder to obtain x-rays. If the x-ray is taken while the patient urinates, it is called a voiding cystourethrogram.
Minimally Invasive Treatment Options for BNC
The primary treatment for BNC is urethral dilation. This nonsurgical procedure involves inserting tubes of increasing diameter through the urethra to gradually widen it, allowing a urinary catheter to be placed. The catheter is then used to drain urine from the bladder.
If you are experiencing urinary issues such as reduced flow or difficulty urinating, the UCI Pelvic Health Center can help. Our specialists offer comprehensive diagnosis and effective treatment for bladder neck contracture.

